PDL1 and PD1
- Discussion
- Referenes
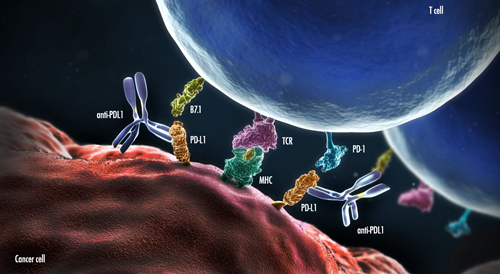
The PD-1/PDL-1 pathway is a key immune checkpoint responsible for downregulation of T cell activation. Since some cancers can have multiple genetic alterations and produce numerous antigens, they may eventually become resistant to the endogenous immune system. PD-1/PDL-1 pathway is an example of an immune checkpoint where some tumors protect themselves from immune destruction by preventing T cells from being activated and attacking the tumor cells. This observation has led to the development of immune checkpoint pathway inhibitors, such as anti-PD-1 and PDL-1 therapies.
Programmed cell death 1 (PD-1), a transmembrane protein, is a crucial immune inhibitory receptor that mediates immunosuppression during inflammation by T cell inhibition, thus preventing autoimmunity. It is expressed by activated T cells, particularly cytotoxic T cells, a subset of B cells in the germinal centers, natural killer cells, dendritic cells, macrophages, and host tissues. It binds to two immunosuppressive ligands, programmed death ligand 1 (PDL-1) and programmed death ligand 2 (PDL-2), that are produced by the immune system in response to inflammation. PDL-2 is expressed mainly on macrophages and dendritic cells. PDL-1 is expressed on immune cells, including T cells, B cells, macrophages, mast cells, and dendritic cells, as well as non-immune cells such as endothelial cells and epithelial cells. In normal tissue, the interaction between PD-1 and PDL-1 is useful, because it prevents excessive activation of immune cells, which could potentially lead to autoimmunity.
In addition to immune cells and normal host tissues, numerous tumor types have also been shown to express PDL-1. In PDL-1-expressing tumoral tissue, PD-1 is upregulated in tumor-infiltrating T cells and PDL-1 is upregulated by tumor cells. In the tumor milieu, the interaction between PD-1 and PDL-1 hampers the immune system’s anti-tumor activity facilitated by PD-1-expressing T cells. This interaction suppresses T cell function and response, preventing T cells from destroying tumor cells. It also inhibits cytokine production and causes apoptosis of tumor-infiltrating T cells. Blockade of the interaction between PD-1 and PDL-1 has been shown to improve T-cell response and anti-tumor activity. It increases the infiltration of cytotoxic T cells into the tumor and promotes T cell activation. Therefore, some patients with PDL1-positive tumors benefit from monoclonal antibody therapies against PD-1 or PDL-1.
Expression of PDL-1 can be ascertained by immunohistochemical analysis performed on formalin-fixed, paraffin-embedded tissue. Results of PDL-1 immunohistochemistry are typically reported as overall percentage of tumor cells, which show any degree of membranous staining. These results are then used to determine eligibility for anti-PDL-1 and anti-PD-1 therapies.
Multiple tumor types have been studied for possible anti-PDL-1 and anti-PD-1 therapies. Some of them include melanoma, non-small cell lung carcinoma, renal cell carcinoma, and pancreatic adenocarcinoma.
Currently, there are two anti-PDL-1 therapies that have been FDA-approved for cancer treatment. KEYTRUDA® (pembrolizumab) is an anti-PDL-1 therapy for patients with non-small cell lung cancer whose tumors show expression of PDL-1 by immunohistochemistry. OPDIVO® (nivolumab) is an FDA-approved anti-PDL-1 therapy for non-squamous non-small cell lung cancer and melanoma.
To date, immunotherapy has shown promising results for treatment of malignancies. Research proposes that combination therapies, such as chemotherapy followed by delayed immunotherapy, may also show positive outcomes for patients with PDL-1-positive tumors. As research on PDL-1 continues, there may be increased development and utilization of anti-PDL-1 and anti-PD-1 therapies for treatment of many different tumor types.
Programmed cell death 1 (PD-1), a transmembrane protein, is a crucial immune inhibitory receptor that mediates immunosuppression during inflammation by T cell inhibition, thus preventing autoimmunity. It is expressed by activated T cells, particularly cytotoxic T cells, a subset of B cells in the germinal centers, natural killer cells, dendritic cells, macrophages, and host tissues. It binds to two immunosuppressive ligands, programmed death ligand 1 (PDL-1) and programmed death ligand 2 (PDL-2), that are produced by the immune system in response to inflammation. PDL-2 is expressed mainly on macrophages and dendritic cells. PDL-1 is expressed on immune cells, including T cells, B cells, macrophages, mast cells, and dendritic cells, as well as non-immune cells such as endothelial cells and epithelial cells. In normal tissue, the interaction between PD-1 and PDL-1 is useful, because it prevents excessive activation of immune cells, which could potentially lead to autoimmunity.
In addition to immune cells and normal host tissues, numerous tumor types have also been shown to express PDL-1. In PDL-1-expressing tumoral tissue, PD-1 is upregulated in tumor-infiltrating T cells and PDL-1 is upregulated by tumor cells. In the tumor milieu, the interaction between PD-1 and PDL-1 hampers the immune system’s anti-tumor activity facilitated by PD-1-expressing T cells. This interaction suppresses T cell function and response, preventing T cells from destroying tumor cells. It also inhibits cytokine production and causes apoptosis of tumor-infiltrating T cells. Blockade of the interaction between PD-1 and PDL-1 has been shown to improve T-cell response and anti-tumor activity. It increases the infiltration of cytotoxic T cells into the tumor and promotes T cell activation. Therefore, some patients with PDL1-positive tumors benefit from monoclonal antibody therapies against PD-1 or PDL-1.
Expression of PDL-1 can be ascertained by immunohistochemical analysis performed on formalin-fixed, paraffin-embedded tissue. Results of PDL-1 immunohistochemistry are typically reported as overall percentage of tumor cells, which show any degree of membranous staining. These results are then used to determine eligibility for anti-PDL-1 and anti-PD-1 therapies.
Multiple tumor types have been studied for possible anti-PDL-1 and anti-PD-1 therapies. Some of them include melanoma, non-small cell lung carcinoma, renal cell carcinoma, and pancreatic adenocarcinoma.
Currently, there are two anti-PDL-1 therapies that have been FDA-approved for cancer treatment. KEYTRUDA® (pembrolizumab) is an anti-PDL-1 therapy for patients with non-small cell lung cancer whose tumors show expression of PDL-1 by immunohistochemistry. OPDIVO® (nivolumab) is an FDA-approved anti-PDL-1 therapy for non-squamous non-small cell lung cancer and melanoma.
To date, immunotherapy has shown promising results for treatment of malignancies. Research proposes that combination therapies, such as chemotherapy followed by delayed immunotherapy, may also show positive outcomes for patients with PDL-1-positive tumors. As research on PDL-1 continues, there may be increased development and utilization of anti-PDL-1 and anti-PD-1 therapies for treatment of many different tumor types.
References
Ji et al. PD-1/PDL-1 pathway in non-small cell lung cancer and its relation with EGFR mutation. Journal of Translational Medicine (2015) 13:5 DOI 10.1186/s12967-014-03730
Kim et al. Prospects for targeting PD-1 and PDL-1 in various tumor types. http://www.cancernetwork.com
Topalian, et al. Targeting the PD-1/B7-H1(PDL-1) pathway to activate anti-tumor immunity. Current Opinion in Immunology 2012, 24:207-212
Nomi et al. Clinical significance and therapeutic potential of the programmed death-1 ligand/programmed death-1 pathway in human pancreatic cancer. Clinical Cancer Research 2007;13(7):2151-2157.
Ji et al. PD-1/PDL-1 pathway in non-small cell lung cancer and its relation with EGFR mutation. Journal of Translational Medicine (2015) 13:5 DOI 10.1186/s12967-014-03730
Kim et al. Prospects for targeting PD-1 and PDL-1 in various tumor types. http://www.cancernetwork.com
Topalian, et al. Targeting the PD-1/B7-H1(PDL-1) pathway to activate anti-tumor immunity. Current Opinion in Immunology 2012, 24:207-212
Nomi et al. Clinical significance and therapeutic potential of the programmed death-1 ligand/programmed death-1 pathway in human pancreatic cancer. Clinical Cancer Research 2007;13(7):2151-2157.

